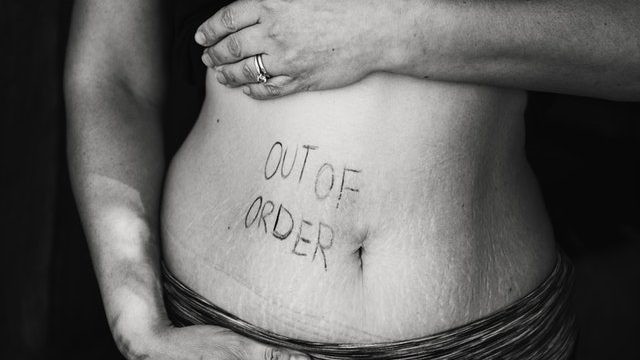
It is common in women that menopause can lead to various problems related to the urinary tract. Menopause and urinary symptoms are some of those issues.
They can be mild to very distressing and even embarrassing, thereby affecting the quality of life considerably.
Menopause And Urinary Symptoms
- It leads to the reduction and then complete cessation of estrogen production. This leads to atrophy of the urinary and the vaginal tract.
- Lack of estrogen leads to loss of the elasticity of the lining. The bladder is not able to stretch enough to hold the urine. Therefore, the woman may want to pass urine at short intervals leading to frequency.
- As they have a sudden urge to pass urine, they also have urgency. A feeling that they will leak in case they do not reach the washroom in time.
- Menopause also weakens the pelvic floor, and this leads to prolapse. Bladder control is compromised, and menopause leads to various types of incontinence issues.
- Lack of estrogen also impacts the pH and reduces the acidity of the tract and increases the susceptibility to bacterial and fungal infections.
- The vagina becomes very dry and therefore there is itching and severe pain during intercourse.
Management Of Vaginal Atrophy
The first step is to ensure there is no infection and in case there is then it is treated with adequate antibiotics.
Hormonal therapy is highly effective in managing the symptoms to a certain extent.
Local estrogen is highly effective in relieving the symptoms of vaginal dryness and pain during sex.
It can also help urinary urgency, frequency, and stress incontinence, and can also help prevent recurrence of urinary tract infections.
Systemic HT also has a role, but the pros and cons need to be discussed with the patient and then take a decision.
Managing Urinary Frequency And Urgency
This involves:
- Life style changes, such as weight control, reduction in caffeine intake.
- Treatment of infection, and good control of comorbidities such as diabetes.
- Behavioural therapy (Biofeedback training)- Bladder-training techniques that increase the capacity to hold urine and control the timing of urination. This is done with the help of a machine.
- Physiotherapy can help with Pelvic floor strengthening exercises.
- Electrical stimulation of the bladder muscles is also used with mixed results.
- Various medicine (antimuscarinic agents, eg. darifenacin, oxybutynin, solifenacin, tolterodine,) have been used with good results.
- They may achieve continence and improve the quality of life.
- But can have some side effects such as urinary retention, dry mouth, constipation, nausea, blurred vision, tachycardia, and confusion.
- Various surgical techniques are available to help with bladder control and these have to be considered after a discussion with the urogynecologist.
Urinary Incontinence
Urinary incontinence is the involuntary leakage of urine.
There are five different sub-types of urinary incontinence:
Stress Incontinence
Leaking of small volumes of urine while coughing sneezing and in worse cases with the change of position. e.g. standing from sitting position.
Management includes behavioral therapy, medication such as Duloxetine, and various surgical procedures.
Urgency Incontinence
As discussed above.
Mixed Incontinence
Most women will have mixed urgency and stress incontinence and therefore a combination of treatment methods is used.
Overflow Incontinence
This is mainly due to neurological problems.
True Incontinence
Continuous leakage as in a case of fistula from the urinary tract to the vagina. This will require surgical intervention.